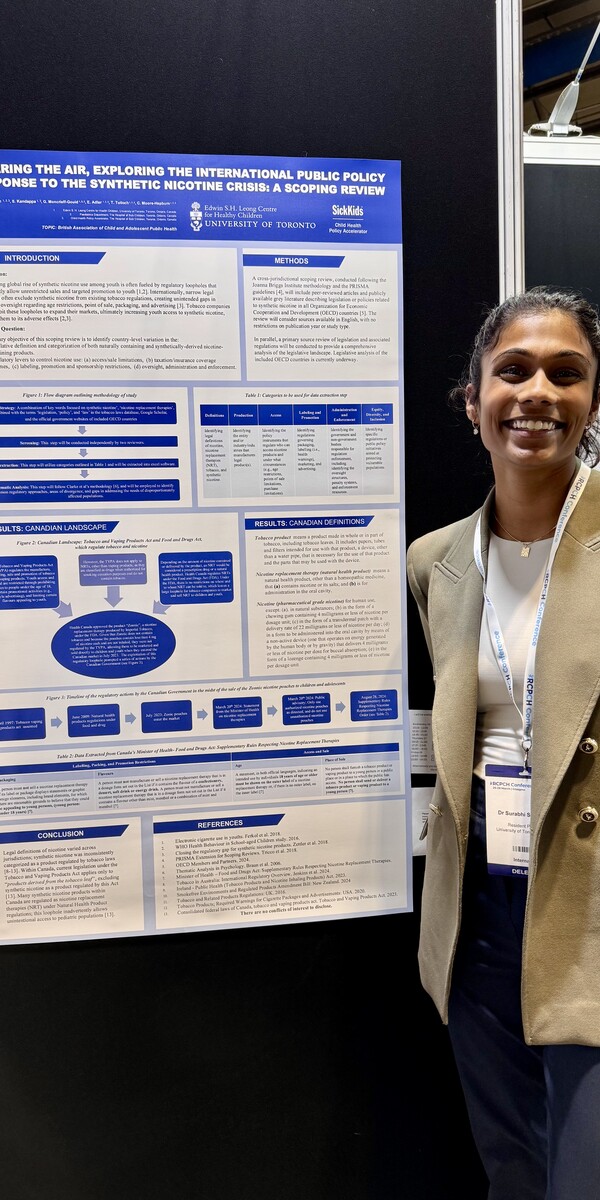
Surabhi Sivaratnam, a second-year pediatric resident at the University of Toronto, presented her research at the Royal College of Paediatrics and Child Health Conference in Glasgow, Scotland (March 2025). Her project examines how federal legislative gaps around synthetic nicotine products increase health risks for youth. Supported by the Edwin S.H. Leong Centre for Healthy Children Studentship Award, her work aims to inform future legislation and advocate for stronger policies to protect children and adolescents in Canada and beyond. A summary of her research is outlined below.
The alarming global rise of synthetic nicotine use among youth is fueled by regulatory loopholes allowing unrestricted sales and targeted promotion to minors [1,2]. Internationally, narrow legal definitions exclude synthetic nicotine from existing tobacco regulations, leaving these products under-regulated or unregulated in terms of age, point of sale, and marketing [3]. These regulatory loopholes inadvertently allow youth access to these high-risk products exposing them to the adverse effects of synthetic nicotine [2,3].
Our project, Clearing the Air, is a cross-jurisdictional scoping review investigating how synthetic nicotine is defined in legislation and regulated across Organization for Economic Cooperation and Development (OECD) countries, with a focus on pediatric-specific safeguards.
To date, our team has conducted a comprehensive analysis of six OECD countries: Canada, Australia, New Zealand, the United States, Ireland, and the United Kingdom. Preliminary findings reveal considerable inconsistencies in how synthetic nicotine is categorized and controlled. For instance, in Canada, nicotine pouches were initially marketed under Natural Health Product regulations, exempting them from tobacco legislation and allowing them to be sold in convenience stores, accessible without age restrictions [4]. This led to emergency advisories and regulatory reforms by Health Canada [5], underscoring the urgency of robust, future-facing policy. While Australia prohibits the sale of nicotine pouches without a prescription, enforcement remains a challenge [6,7,8]. In New Zealand, synthetic nicotine is regulated as a pharmacy-only medicine, under the Medicines Regulations 1984 [9], and oral nicotine products cannot be legally imported for personal or retail use unless approved as a medicine [10]. Despite these regulations in New Zealand, synthetic nicotine pouches continue to be available through informal online markets [11]. There is an urgent need for Canada to explore and learn from other jurisdictions, to build and apply the best public policy interventions to close gaps that industry exploits.
We shared early insights from our work at the Royal College of Paediatrics and Child Health (RCPCH) Conference in March 2025. The presentation received enthusiastic engagement from pediatricians, respirologists, and child health advocates from around the world, all emphasizing the need for international cooperation and youth-focused regulation.
In the coming months, we will finalize our analyses for the remaining English-speaking OECD countries and complete our thematic analysis. Findings will inform a peer-reviewed manuscript and we aim to meet with politicians and policymakers advocate for change, aiming to protect children and youth from exposure to synthetic nicotine.
This work is proudly led by the Edwin S.H. Leong Centre for Healthy Children and the Child Health Policy Accelerator at the Hospital for Sick Children. Together, we are committed to safeguarding youth health in an evolving global nicotine landscape.
References: